Several changes have been made between the 2021 Star Ratings and the 2022 Star Ratings; below is a summary of key measure and methodological changes, as well as the impact they may have on your plan.
Key Changes for Star Year 2022
For 2022 Star Ratings, the underlying data for HEDIS and CAHPS measures will resume use of the most recent available dataset.
- However, historic data will remain in play for measures where the “greater-of” logic results in the use of your prior year’s measure data (Star Year 2020 for HEDIS and CAHPS).
Mean resampling was added to the hierarchical clustering methodology that is used to set cut points for non-CAHPS measures.
- Mean resampling will reduce the sensitivity of the clustering algorithm to outliers by reducing the random variation that contributes to cutpoint fluctuation, increasing stability over time. This is the first of a series of methodological enhancements CMS is implementing over a three year period in effort to stabilize cut points. Cut point data from Star Year 2022 will also be used to establish a baseline for the implementation of cut point guardrails, effective Star Year 2023. As a reminder, the guardrail will be a bi-directional cap that imposes a 5% maximum allowable movement from the previous year’s cut points for each measure threshold, allowing for some degree of predictability.
The Re-specified MPF Price Accuracy measure moved into the 2022 Star Ratings as a new measure.
- As a “new measure”, CMS will calculate each contract’s overall rating “with” and “without” including the new MPF Price Accuracy measure. They will apply whichever calculation results in the higher rating for your contract.
For 2022 Star Ratings only, CMS expanded the existing quality improvement (QI) measure hold harmless provision to all contracts at the overall and summary rating levels.
- Note that contracts do not have the option of reverting to the prior year’s QI rating. Additionally, any of your contract’s measures that reverted back to previous year’s Star Rating (due to the application of the “greater-of” logic) are excluded from the QI measures calculation.
For 2022 Star Ratings only, the disaster policy was modified to remove application of the 60% rule and avoid the exclusion of contracts with 60% or more of their enrollees living in FEMA-designated Individual Assistance areas from calculation of both the non-CAHPS measure-level cut points and the Reward Factor.
- As mentioned in yesterday’ s blog, it is important that your plan calculates both individual measure performance and overall contract performance with and without application of these one-time COVID related modifications. Failure to recognize true performance honestly and openly will only mask performance decline, pushing the mounting consequences of failure-to-act down the road.
Measures Being Temporarily Moved to Display:
Because NCQA made substantive changes to the measure specification the Care of Older Adults – Functional Status Assessment, the measure was temporarily moved to the display page for the 2022 and 2023 Star Ratings. Improving or Maintaining Physical Health and Improving or Maintaining Mental Health made an earlier than expected move to the display page due to validity concerns related to the public health emergency. We won’t see these HOS outcomes measures again until Star Year 2026! That said, we encourage your plan to keep these measures in the workplan. Due to the retrospective nature of Stars, performance rates and ratings will already be ‘baked’ when these measures return in Star Year’s 2024 and 2026, respectively.
Measures Being Permanently Retired from the Ratings:
Adult BMI and the two Part D appeals measures are now permanently retired from the ratings.
Star Year 2022 Cut Point Analysis:
Star Year 2022 cut points were filled with some expected results as well as some surprises. Following, is a breakdown by functional area.
CAHPS:
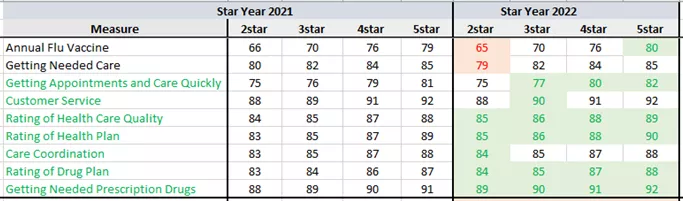
As mentioned in my previous article we saw a significant, across the board increases in CAHPS cut points this year, with only two measures at the 2-Star threshold declining. To be fair, we would expect Getting Needed Care and Annual Flu Vaccine to be more challenging to improve in the midst of a pandemic. All other cut points either maintained or, in most cases, shifted to the right. Most likely a testament to the many health plans that went out of their way to ensure their members felt as supported and healthy as possible throughout 2020 and into 2021.
HEDIS:
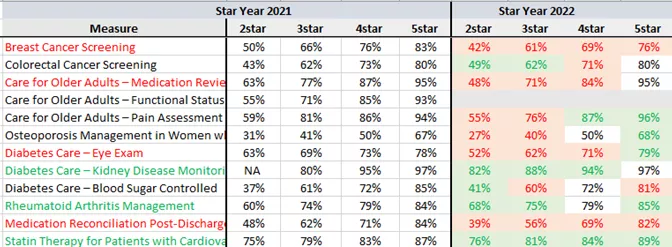
I am sure that few plans were surprised to see a significant shift to the left for measures like Breast Cancer Screening and CDC Eye Exam, where COVID-related obstacles made gap closure next to impossible. On the other hand, for gaps that could be closed via non-traditional care delivery methods such as in-home test kits and telehealth, we see a shift to the right (e.g., CDC Kidney Disease Monitoring, Colorectal Cancer Screening, Statin Therapy for Patients with Cardiovascular Disease).
With COVID mutations entering the scene and a number of Americans yet to be vaccinated, plans would be wise to continue (and to build upon) many of these new and modified approaches to gap closure, including working closely with provider partners to improve access to telehealth services and in-person care for their most vulnerable subsets of members. Also, plans should continue to educate members on the importance of wearing a mask in public-indoor places, using hand sanitizer, social distancing, and most importantly, getting their COVID vaccinations and subsequent boosters. As a reminder, CMS solicited feedback from plans through recent regulatory guidance (including the calendar year 2022 Advance Notice) and on several different measurement concepts for stars, including COVID-19 Vaccination measures.
HOS:
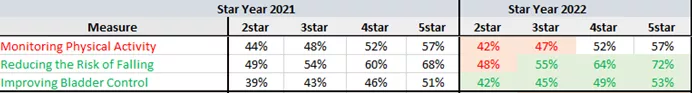
Star Year 2022 HEDIS/HOS ratings data come from the combined results of the cohort 23 baseline survey (fielded in calendar year 2020) and the cohort 21 follow-up survey (also fielded in CY 2020). Due to COVID, the fielding of these surveys (which historically occurred in the Spring) was delayed until August. However, because the questions ask members about activities and conversations that took place over the last 12 months (into CY 2019), CMS will not apply the greater-of logic to these measures until Star Year 2023.
Plans have made notable improvements in Reducing the Risk of Falling and Improving Bladder Control, with both measures displaying nearly across-the-board cut point increases at every threshold. Monitoring Physical activity leaves room for improvement. Even though the disaster policy is not applied to HEDIS/HOS this Star year, one can’t help but wonder if having a captive audience for HOS messaging via telehealth, IHAs, educational calls and mailers had some impact on Falls & Bladder.
Pharmacy
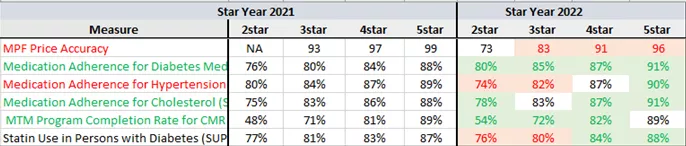
Those of us that spend our free time studying the national average ratings in health plan Acumen data may have seen the cut point increases coming for the medication adherence and SUPD measures. For the rest of you, this may have come as a surprise.
We suspect that increased efforts to ensure members received needed medications during the pandemic impacted this shift to the right. Many of our clients invested heavily in direct-to-member outreach efforts, 90 to 100-day prescription fills, mail-order pharmacy, and courier drug delivery services. If your plan has not been focusing on the pharmacy measures, you have one more quarter left in the measurement year to try to make up for lost time, and at a minimum, you should focus efforts on Part D improvement plans for the calendar year 2022/Star year 2023.
Also noteworthy is the impact that the two-part D appeals measures permanently retiring from the ratings will have on the five-times-weighted Part D Quality Improvement measure. High performance in this measure is now dependent on the statistically significant improvement of an even smaller subset of measures, making improved Part D performance even more meaningful to a plan’s overall rating!
Admin/Operational:
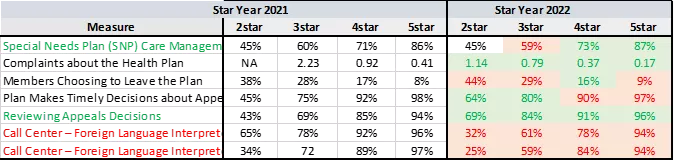
This was a year for dramatic cut-point swings in the operational measures. Clearly, there were less members calling 1-800-Medicare to complain about their plan, possibly a reflection of improved health plan customer service efforts both in response to COVID and the continuing increase in weight being placed on member experience.
However, this was not the case for the Members Choosing to Leave the Plan measure. Deft’s annual report on MA shopping and switching provides some insights on the impacts of the COVID-19 pandemic and the general election on beneficiary’s health insurance experience. Results of the study call out dissatisfaction with dental benefits, poor health plan customer service and supplemental benefit offerings as the key motivating factors for plan switching/disenrollment. We will definitely be on the look out for more research based studies in this space!
For the Part C Reviewing Appeals Decisions measure, we also see a shift to the right at every cut point threshold. Possibly due to looser UM criteria and increased/expanded service coverage in response to COVID, leaving less for members to appeal?
Maybe most noteworthy is the significant shift to the left (at every cut-point threshold) for the two, soon to be four times weighted, call center FLL/TTY Star measures. A number of our clients disputed their call center measure rates this year and, as called out in yesterday’s HPMS memo announcing the 2nd PP, call center data were updated for a small number of contracts. Regardless, with all of the measures in this category now dominating the Star Ratings, (especially when combined with CAHPS) now is the time for your plan to put in place strict monitoring practices, a clear accountability structure and issue resolution and escalation pathways.
Next Steps
Are you still confused about your Star Year 2022 results? We are happy to walk you through it step-by-step. Trying to project where you stand with all of the upcoming changes, both codified and proposed, for Star year’s 2023 and beyond? We can help with that too! Need some help updating your work plan to include best-in-class interventions and strategies…you get the idea, give us a call!




