The Centers for Medicare & Medicaid Services’ (CMS’) recently released final rule finalized changes to the Medicare Advantage (MA) prescription drug program (MA-PD) for Contract Year 2025 (CY 2025). CMS’ stated goal for the final rule is to strengthen consumer protections and guardrails, promote fair competition, and ensure MA and Part D plans can best meet the healthcare needs of Medicare beneficiaries, including those dually eligible for Medicaid and Medicare.
The final rule is wide-reaching and will require plans to make changes to operations and strategy across many health plan functions. We previously published a brief on the final rule’s policies impacting broker and agent compensation. This brief focuses on new rules related to CMS’ desire to create greater integration between Medicare and Medicaid services for those enrolled in Dual Special Needs Plans (D-SNPs).
What Issue is CMS Trying to Solve?
Dually eligible beneficiaries navigate a complex landscape of plan choices. Many of these coverage options, including D-SNP, often do not integrate Medicare and Medicaid benefits because the parent organization offering the D-SNP plan may not also deliver enrollees’ Medicaid services.
Existing managed care enrollment and eligibility policies (e.g., quarterly Special Enrollment Periods) have resulted in a proliferation of D-SNPs, leaving dually eligible individuals susceptible to aggressive marketing tactics from agents and brokers throughout the year.
Despite CMS’ efforts to improve beneficiaries’ experience and outcomes through various forms of Medicare-Medicaid integration, a significant portion of dually eligible beneficiaries remain misaligned. This means that beneficiaries receive Medicare services from one managed care entity and Medicaid services from a separate entity (“misaligned enrollment”) rather than one organization delivering both Medicare and Medicaid services (“aligned enrollment”). In the long-term, CMS wants to make aligned enrollment the standard—ideally the only— managed care enrollment scenario for dually eligible beneficiaries. This shift would improve the experience and outcomes for dually eligible beneficiaries and streamline administrative and financial processes for CMS and state Medicaid agencies.
What Regulations did CMS Finalize?
CMS clarified that it is focused on increasing enrollment in integrated D-SNPs, defined as:
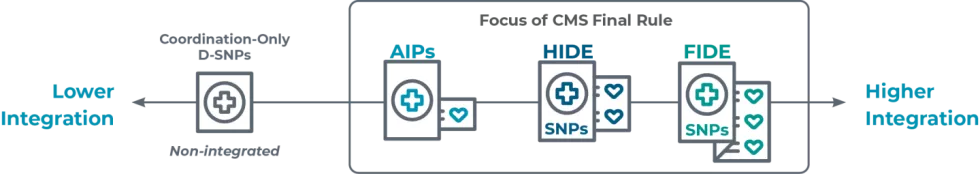
Fully Integrated Dual Eligible Special Needs Plans (FIDE SNPs): D-SNP is required to have Exclusively Aligned Enrollment (EAE). These D-SNPs provide nearly all Medicaid services, including long-term services and supports, Medicaid behavioral health services, home health, and durable medical equipment (DME).
Highly Integrated Dual Eligible Special Needs Plans (HIDE SNPs): Unlike FIDE SNPs, HIDE SNPs are required to cover either LTSS (long-term services and supports) or behavioral health services. However, HIDE SNPs may exclude some additional Medicaid services from their coverage.
Applicable Integrated Plans (AIPs): D-SNPs also require EAE, and the companion Medicaid managed care organization (MCO) typically covers Medicaid benefits. This includes primary care and acute care, Medicare cost-sharing support, and at least one of the following: home health services, DME, or nursing facility services.
To address these issues, CMS has finalized a set of inter-connected policies intended to increase aligned enrollment for beneficiaries enrolled in D-SNPs:
1. Beginning January 1, 2025, the current quarterly Special Enrollment Period (SEP) will be replaced with:
- Monthly SEP for dually eligible individuals and other Low Income Subsidy (LIS) eligible individuals to opt-out of D-SNP and elect a standalone Medicare Prescription Drug Plan (PDP) (essentially reverting back to traditional Medicare fee for service).
- New, monthly integrated care SEP allows dually eligible individuals to elect an integrated D-SNP (e.g., FIDE, HIDE, or AIP with the same parent Medicaid MCO as the D-SNP plan).
CMS clarified that they are finalizing a narrower scope for the integrated care SEP than in the proposed rule to facilitate aligned enrollment. This SEP allows dually eligible beneficiaries to switch to a FIDE SNP, HIDE SNP, or AIP only if they are already enrolled in, or applying for, the sponsor’s affiliated Medicaid managed care plan.
2. Starting January 1, 2027, when a MA parent organization also contracts with the state as a MCO that enrolls dual eligibles in the same service area, D-SNPs must limit new enrollment to individuals enrolled in the D-SNP’s affiliated Medicaid MCO.
Interestingly, this policy would not have a negative impact on D-SNPs that do not offer Medicaid in the same service area. CMS clarified that “MA organizations that offer D-SNPs where the MA organization, its parent organization, or any entity that shares a parent organization with the MA organization do not offer an MCO are unaffected by the new proposals; such MA organizations may continue to offer coordination-only D-SNPs.”
In fact, commenters noted the perverse incentive of penalizing MA plans that are aligned with a Medicaid MCO, while MA plans not aligned with a Medicaid MCO may enroll any individual. CMS acknowledged this potential contradiction but indicates that the SEP change should have a counterbalancing effect that benefits organizations that have aligned enrollment.
3. Beginning January 1, 2027, only one D-SNP may be offered by an MA organization (MAO), its parent organization, or another MAO with the same parent organization in the same service area as the aligned Medicaid MCO.
CMS will only contract with one D-SNP for full-benefit dually eligible individuals in the same service area as that MAO’s affiliated Medicaid MCO. CMS makes limited exceptions, mainly for states with unique Medicaid programs for specific coverage types.
4. Beginning January 1, 2030, D-SNPs can only enroll individuals enrolled in the affiliated Medicaid MCO.
Therefore, by 2030, integrated D-SNPs will be required to disenroll individuals who are not enrolled in both the D-SNP and Medicaid MCO offered by the same parent organization.This policy would have significant impact on organizations that offer D-SNPs but do not participate in the state’s Medicaid managed care program. CMS clarified that the required disenrollment is from the D-SNP (not from the Medicaid MCO). While CMS clarified that disenrollment only applies to the D-SNP (not Medicaid), it acknowledged the potential disruption. However, with a significant lead time until 2030, CMS officials believe D-SNPs have ample opportunity to align more enrollees with their affiliated Medicaid MCOs.
What should health plans do?
The impact of these policies will vary based on how an organization participates in both MA and Medicaid programs.
Figure 1: Strategic Positioning Based on Medicare and Medicaid Program Participation
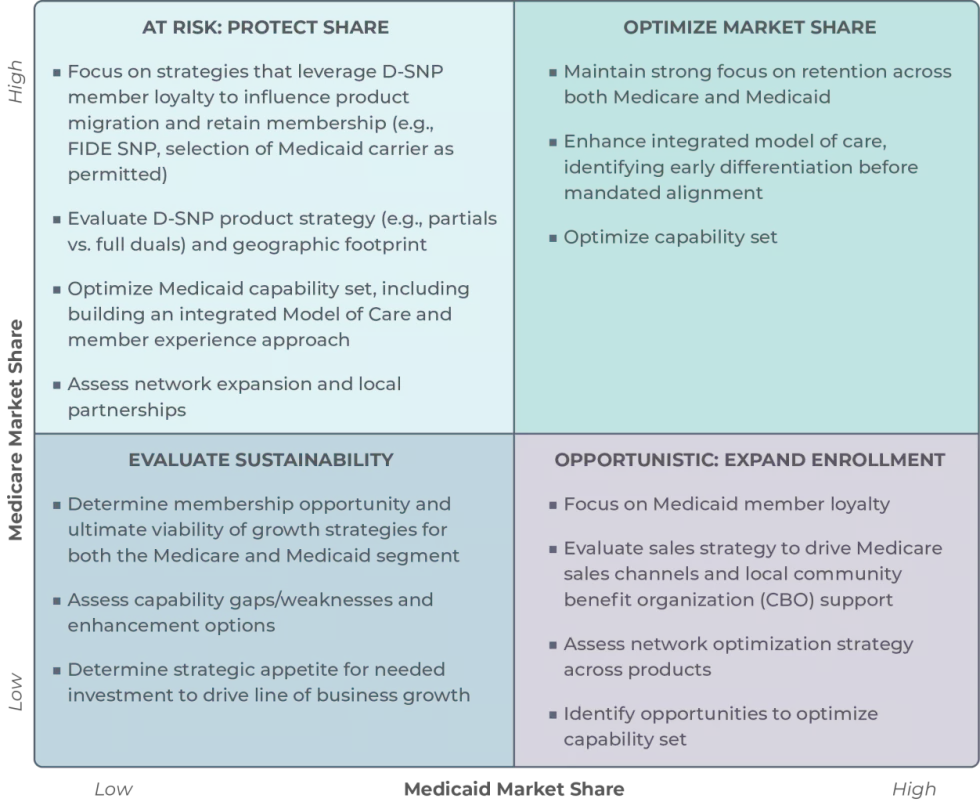
Current enrollment distribution between Medicaid and MA (D-SNP) has implications for plans’ current and future competitive positioning. Regardless of whether the 2025 final rule presents a strategic opportunity or a notable risk to plans, plans should consider the following preparatory actions as they prepare for the changes:
Understand your market: Establish an understanding of your local D-SNP and state Medicaid market landscape to model the implications of the final rule to in-market players. This assessment should inform both strategic direction and investment decisions for plans seeking to prepare for integrated models over the next 3 to 5 years. This assessment should reflect the policies laid out by CMS in the final rule as well as the state regulatory landscape, especially where policy direction may differ.
Determine participation options and size the opportunity: Identify options available for the plan to participate in the dual-eligible market. Conduct enrollment and financial modeling to size the potential impact of these options, considering changes in enrollment, revenue, and medical loss ratio.
Establish a multi-year strategic plan: Confirm strategic options and associated investments to respond to CMS and state regulatory actions. Develop responses for the short-, medium-, and longer- term horizons that reflect CMS milestones and anticipated/known actions from state Medicaid. This planning could also include identifying alternative product options or market participation strategies based on current line of business participation and membership composition.
Shore-up organizational capabilities and partnerships: Define capability gaps and establish a roadmap to address gaps while meeting shifting requirements and improving market competitiveness.
HEALTHSCAPE CAN HELP
The new regulations for D-SNP present both challenges and opportunities for plans and implications vary, depending on an organization’s participation, presence, and capabilities across Medicare and Medicaid. We support plans across the country in both these lines of business, helping them navigate these regulatory and competitive environment changes to achieve a sustainable competitive advantage.




